Living with gastroesophageal reflux disease (GERD) presents unique nutritional challenges, as I, like many others, have learned first-hand. I’ve experienced how an acid reflux diet can significantly impact day-to-day comfort and overall health. Knowing that more than 20% of the population grapples with this, I’ve found it imperative to understand which foods for acid reflux can provide relief from the persistent heartburn and discomfort associated with this condition.
As I dove deeper into the world of GERD-friendly nourishment, it became clear that certain choices could spell the difference between agony and relief. The unwelcome sensation of heartburn, that all-too-familiar burning in the throat and chest, can often be mitigated with thoughtful dietary adjustments. By incorporating foods to help with acid reflux into my regimen, I’ve managed to alleviate some of the distress these symptoms cause.
While there is no one-size-fits-all acid reflux diet, familiarizing myself with the types of food that can either trigger or relieve the symptoms of acid reflux became a stepping stone toward finding my personal heartburn relief.
- A well-planned GERD diet can considerably reduce the symptoms of acid reflux.
- Identifying and incorporating foods for acid reflux can lead to significant heartburn relief.
- It is crucial to avoid known triggers such as fried foods, spicy ingredients, and certain beverages.
- Implementing a diet rich in alkaline foods and whole grains can help neutralize stomach acid.
- Staying informed about the foods to help with acid reflux is key for managing GERD effectively.
Understanding GERD and Its Dietary Implications
As someone who has navigated the challenges of living with GERD, I can attest to the profound impact that diet can have on managing this condition. An understanding of how certain foods interact with our bodies is critical for those of us seeking to quell the uncomfortable symptoms of acid reflux. Through mindful eating and specific dietary changes, I’ve learned it’s possible to live a life not defined by this condition.
Defining Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease, known simply as GERD, occurs when stomach acid makes its unwelcome return to the esophagus. This backflow, which should be a one-way street, leads to the irritation and burning sensations that plague me and many others. Immediate harm aside, the long-term effects of this acid incursion can cause lasting damage to the esophageal lining, emphasizing the need for effective management strategies.
The Role of Diet in Managing Acid Reflux
My journey with GERD has taught me the power of dietary choices. Foods that are high in acid or fat can relax the lower esophageal sphincter—the gatekeeper between the stomach and esophagus—thereby delaying digestion and exacerbating reflux symptoms. Incorporating gerd friendly foods and understanding what to eat for acid reflux has become second nature to me. This deliberate approach to managing GERD dietary changes has proven instrumental in keeping my symptoms at bay.
How GERD Affects Daily Life and Eating Habits
Living with GERD goes beyond occasional discomfort; it has a tangible impact on daily life and requires constant vigilance with eating habits. As someone who values food and the pleasures of eating, I’ve had to adapt by striking a balance between enjoying meals and preventing the all-too-familiar burn of acid reflux. It’s a dynamic process that involves learning from each experience and making modifications as needed. By staying informed and agile, I’ve managed to turn managing GERD into a journey of dietary discovery rather than a restrictive regimen.
Discovering which foods soothe or fuel the fiery symptoms of GERD has been a transformative personal project. With each bite, I’ve gained insight into how my body reacts, which has been as educational as it is beneficial to my health.
The Science Behind Acid Reflux Relief
As someone who has dealt with the nagging discomfort of GERD, I have become increasingly attuned to the dietary approaches that can encourage acid reflux relief. The dynamic relationship between the foods we choose to eat and the occurrence of heartburn has become a central focus of my daily nutrition. In pursuit of heartburn relief, I’ve learned that certain foods have the innate ability to diminish the harshness of reflux episodes, which can greatly improve quality of life for those like myself dealing with GERD.

How Certain Foods Alleviate GERD Symptoms
Experience has taught me that alkaline foods are vital in managing acid levels in the stomach. By incorporating such foods—melons, bananas, and avocados to name a few—into my diet, I can effectively counteract the acidity that leads to the irritation and pain characteristic of GERD. Moreover, snacking on nuts or adding a generous helping of spinach to a meal can grant unanticipated respite from acidity. Beyond quelling immediate symptoms, these dietary changes have also had a lasting impact on my overall digestive wellbeing.
The Relationship Between Food Choices and Acid Reduction
One does not need to delve into the esoteric of nutrition science to appreciate the benefits of whole grains and hearty vegetables. Stalwarts like couscous, brown rice, and oats stand as bulwarks against the acids that would otherwise provoke GERD’s signature discomfort. Green vegetable siblings—broccoli and green beans—join the fray alongside root vegetables such as beets and sweet potatoes, creating a well-rounded front against indigestion. And let’s not overlook the silent work done by high-water-content foods like cucumbers and watermelons; these hydrating choices along with the soothing presence of herbal teas and broths provide a comprehensive approach to managing GERD symptoms.
GERD Diet: Foods That Help with Acid Reflux
Embarking on a dietary journey to manage my GERD, I’ve come to appreciate the profound relief that certain foods provide. Striving to maintain a selection of safe ingredients for acid reflux, I’ve curated a list of staples I can rely on for comfort and sustenance. Below, I share insights into these beneficial food groups with fellow sufferers looking for alleviation through GERD-friendly eating practices.
The struggle with acid reflux doesn’t solely belong in the domain of medical intervention; dietary choices play a crucial role as well. By incorporating these selections into your meals, you may find solace and symptom reduction, as I have in my ongoing quest for a harmonious digestive health.
Alkaline Foods to Counteract Stomach Acid
Diving into the realm of pH balance, alkaline foods have become my allies against the hostile surge of stomach acid. Consciously consuming high pH foods such as melons, bananas, and avocados has been instrumental in neutralizing my body’s acidity levels. Embracing a plate filled with these options has often led to immediate and noticeable reductions in discomfort.
Identifying GERD-Friendly Foods
The search for GERD-friendly foods has been both an exploration and a delight. Whole grains like quinoa, brown rice, and oats have replaced refined carbs in my pantry. These grains provide a stable energy source without aggravating my symptoms, proving that one need not sacrifice satiety for comfort. The different forms these grains come in also mean a variety of foods for acid reflux are just a recipe away.
What to Eat for Acid Reflux: Safe Ingredients
Understanding what makes for safe ingredients for acid reflux has been a cornerstone of my dietary modification. Non-acidic vegetables and root vegetables—a colorful spectrum ranging from leafy greens to the earthy richness of beets and sweet potatoes—form a crucial part of my meal planning. Their contribution to my well-being goes beyond mere nutrition, offering a buffer against the burn of reflux.
Hydrating foods like cucumbers, watermelon, and celery deliver not just a splash of refreshment, but also a soothing effect on my esophageal walls. And let’s not forget the humble power of low-fat dairy products, particularly milk, which in moderation, can sometimes soften the edge of heartburn’s sharp blade.
Amidst the usual culprits of culinary-induced heartburn, I was surprised to find solace in ginger’s inflammation-reducing qualities and even diluted lemon juice with honey, which can act as a natural antacid when my defenses are down.
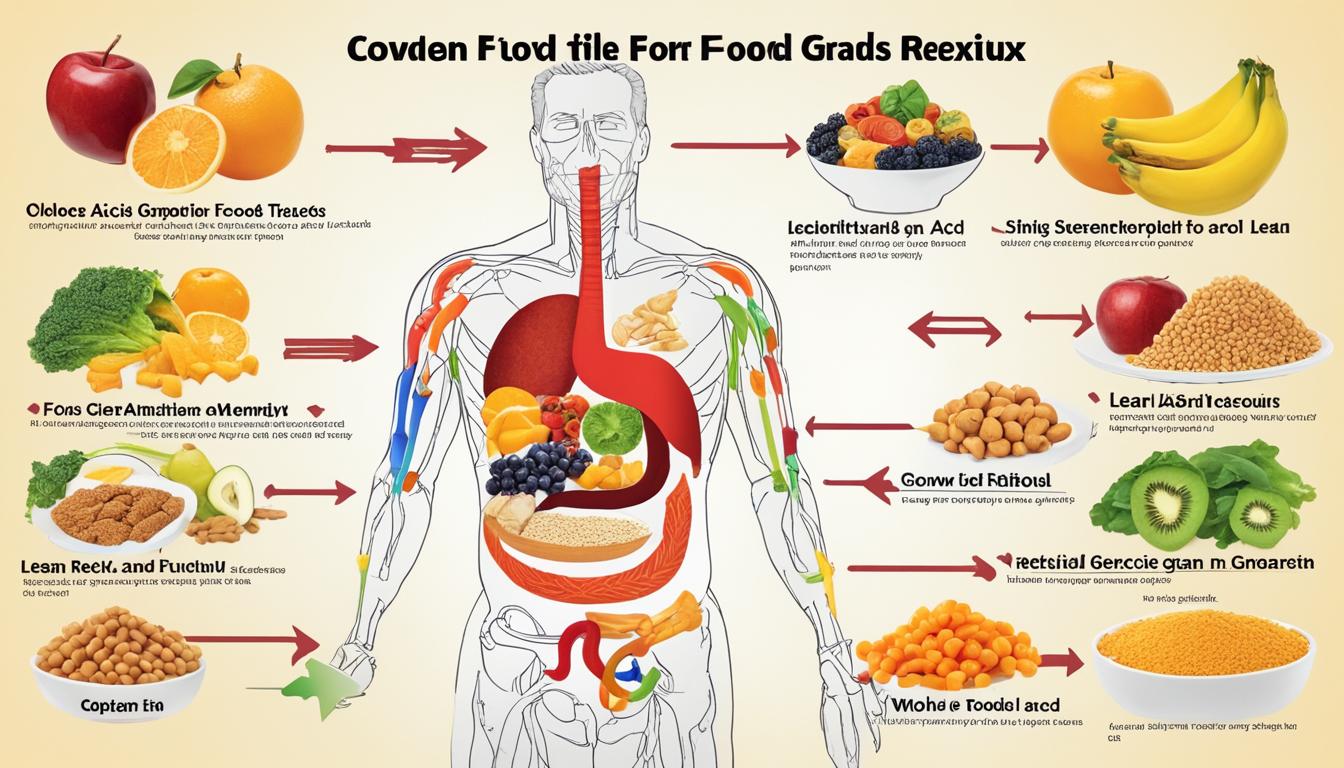
As someone directly affected by GERD, I find that maintaining a diary of dietary reactions helps clarify which foods are truly friends or foes. Crafting meals around these principles not only helps me manage my condition but also enriches my enjoyment of food despite the restrictions GERD imposes. Below is a visual guide I’ve put together to encapsulate the GERD-friendly foods that have made a difference in my life:
| Food Category | Examples | Benefits |
|---|---|---|
| Alkaline Foods | Melons, Bananas, Avocados | Neutralizes stomach acid |
| Whole Grains | Quinoa, Brown Rice, Oats | Provides satiety; low acid impact |
| Vegetables & Roots | Broccoli, Beets, Sweet Potatoes | Rich in nutrients; less likely to cause reflux |
| Hydration-Rich Foods | Cucumbers, Watermelon, Celery | Helps soothe esophageal lining |
| Low-Fat Dairy | Low-Fat Milk, Yogurt | Potential to soothe heartburn |
| Anti-Inflammatory | Ginger, Lemon Juice with Honey | Reduces inflammation; may act as a natural antacid |
Adopting this table as a nutritional compass, I’ve sailed through many a troubled digestive storm. These food groups have been the cornerstone of my GERD management, enabling me to enjoy meals with the confidence that I am nurturing, rather than challenging, my body.
Common GERD Triggers and Foods to Avoid
When managing my GERD symptoms, identifying and sidestepping certain food items has been fundamental to avoiding GERD symptoms. Through trial and error, I’ve learned that certain foods act as acid reflux triggers, leading to painful flare-ups and discomfort. Here, I aim to share my insights on avoiding these triggers and fostering a more comfortable everyday life.

The Consequences of Eating Trigger Foods
Ignoring the potential impact of trigger foods is akin to inviting distress. Consuming foods known to exacerbate GERD has led me to experience a range of symptoms, from intense heartburn to lingering discomfort. These acid reflux triggers can compromise my esophageal lining over time, making the identification and avoidance of such foods a health priority for me.
Foods Known to Worsen Acid Reflux Symptoms
In my path to alleviating GERD symptoms, I’ve pinpointed a series of problematic foods. Fried and fatty foods, for instance, have been reliable culprits in triggering my acid reflux. Spicy dishes laden with cayenne and black pepper wreak havoc on my digestive peace, while acidic foods like tomatoes and citrus fruits prove to be just as problematic. I’ve found that high-fat dairy and decadent chocolate fall squarely into the list of items to avoid in my GERD diet.
Understanding Food Intolerances Related to GERD
GERD, I’ve learned, isn’t a one-size-fits-all condition. Food intolerances play a significant role in understanding and managing the disorder. While the general list of problematic foods is a helpful starting point, I’ve discovered, through careful observation, my personal sensitivities in this context. This individualized approach to acknowledging food intolerances in GERD has allowed for a nuanced management of my symptoms, significantly aiding in avoiding GERD symptoms and improving my quality of life.
Through consistent monitoring and adapting my diet to sidestep these triggers, I’ve successfully circumvented many of the pitfalls that used to derail my digestive health. By sharing these experiences, I hope to encourage fellow GERD sufferers to also recognize and respect their body’s responses to certain foods, fostering a lifestyle tailored to their personal needs.
Digestive Health and Lifestyle Enhancements for GERD
As someone who experiences GERD firsthand, I’ve come to realize that controlling symptoms extends beyond the realm of food choices and into the territory of whole-life adjustments. It’s not just about what I eat, but also how I weave digestive health into my daily routine that makes all the difference.
The Importance of Meal Timing and Frequency
One key aspect that I’ve had to adjust is meal timing for acid reflux. By breaking down my food intake into smaller, more frequent meals, I’ve noticed a considerable easing of symptoms. This method allows my stomach to handle only a limited amount of food at a time, reducing the likelihood of an acid onslaught.
The discipline extends to not just daytime meals but also to my evening eating habits. Waiting at least two to three hours before heading to bed gives my system much-needed time to digest, thereby minimizing the risk of a nocturnal reflux episode.
Impact of Sleep and Gravity on Acid Reflux
The forces of nature, namely gravity, play a role in my struggle against acid reflux. Sleep positions matter; elevating the head of my bed provides a subtle incline which helps keep stomach contents where they belong. With acid naturally succumbing to gravity’s pull, my esophagus gets a reprieve during the most vulnerable time—when I am lying down to rest.
| Bedtime Habit | Benefit |
|---|---|
| Head Elevation | Reduces Esophageal Pressure |
| Left-side Sleeping | Enhances Gravity’s Effect |
| Avoiding Late Meals | Lessens Nighttime Reflux |
Stress Management and Physical Activity Considerations
In managing my GERD symptoms, stress has emerged as a factor that can’t be ignored. High stress levels have a sneaky way of exacerbating reflux, thus making relaxation techniques a part of my routine for fostering digestive health. Adjusting my approach to physical activity also had an impact; avoiding strenuous exercises right after meals has made my workouts more GERD-friendly.
Maintaining calm and staying active without crossing the line into an intensity that triggers reflux is a delicate balance—one that requires mindfulness and adaptation.
Facets of life as mundane as sleep positioning or as intrinsic as stress management may seem distant from the direct sphere of GERD lifestyle changes, yet I’ve learned they are closely intertwined. Such adaptations not only ease the physical symptoms but also provide a sense of control over a condition that can often feel unpredictable and unmanageable.
Creating a Personalized GERD Diet Plan
My personal struggle with GERD has highlighted the importance of a diet plan that is as unique as the symptoms I experience. Tailoring my diet to address acid reflux has not only provided comfort but has also become a crucial aspect of my everyday health regimen.
Consulting Healthcare Professionals for Tailored Advice
Engaging with specialized healthcare providers has been a vital step in constructing a personalized GERD diet plan. These professionals, often gastroenterologists, offer a wealth of knowledge regarding which foods could trigger my reflux symptoms and alternative dietary suggestions. Their expertise extends to navigating potential medical treatments that can work in tandem with diet to manage GERD effectively.
Monitoring Symptoms and Adjusting the Diet Accordingly
Meticulous monitoring of acid reflux symptoms has become second nature to me. By keeping a detailed food log and noting the reactions my body has to different foods, I am able to understand which foods alleviate or exacerbate my condition. This ongoing process of observation and modification allows for continuous fine-tuning of my GERD diet to ensure optimal control and comfort.
In my experience, some particular dining habits have made noticeable differences in managing my symptoms. Implementing these personalized adjustments has been empowering, reminding me that I have an active role in alleviating my own discomfort. Here’s a track record of my findings:
| Food or Habit | Impact on Acid Reflux Symptoms | Personal Adaptation |
|---|---|---|
| Alkaline Foods | May reduce acidity and soothe symptoms | Included avocados and bananas in my diet |
| Meal Timing | Reduces likelihood of nighttime reflux | Avoid eating 3 hours before bedtime |
| Monitoring Portion Sizes | Smaller portions minimize pressure on the esophageal sphincter | Opted for frequent, small meals |
| Hydration | Helps digestion and dilutes stomach acid | Increased water intake, especially between meals |
With the guidance of my healthcare team and personal observation, I’ve come to understand the landscape of my condition better. Furthermore, consulting healthcare for GERD and consistent patterns in my diet have fostered an environment in which I can confidently face daily challenges with GERD.
It’s a dynamic and often challenging journey, but it is one that is necessary for those of us looking to live more comfortably with GERD. As someone who lives with this condition, my advice to others is to be patient and persistent. After all, creating a personalized GERD diet plan is a process of trial and error, but it is one that can lead to greatly improved day-to-day health and comfort.
Navigating Challenges and Setbacks in a GERD Diet
Commitment to a GERD-friendly diet is a pivotal part of managing the condition, but it’s not without its hurdles. As someone who has had to navigate this terrain, I know well that unexpected GERD flare-ups can sometimes derail even the most diligent efforts. Moreover, the social and emotional landscape of living with dietary restrictions requires thoughtful navigation to maintain not just physical, but also mental wellbeing.
How to Manage Occasional Flare-Ups
Despite every precaution, managing GERD flare-ups is a reality many of us face. Quick and effective strategies are crucial for mitigating these episodes. I personally have found that maintaining a food diary helps in identifying potential triggers, allowing for swift dietary adjustments. Additionally, keeping a stock of GERD-friendly snacks can prevent reaching for foods that may exacerbate the situation. It’s also essential to have a conversation with your healthcare provider about rescue medications or soothing natural remedies that can be used in a pinch.
Coping with Dietary Restrictions Socially and Emotionally
Dealing with GERD challenges extends to social scenarios, where food is often at the center of gatherings. Understanding and coping with GERD diet restrictions in these settings can be awkward and stressful. Ensuring open communication with friends and family about my dietary needs has been key. When dining out, I make it a practice to scout the menu ahead of time or suggest restaurants that offer GERD-friendly options. Emotionally, connecting with support groups, whether in person or online, provides a space to share experiences and learn from others who understand the journey.
| Challenge | Strategies | Benefits |
|---|---|---|
| Unexpected Flare-Ups | Keep a food diary; Discuss rescue options with your doctor | Reduces severity and duration of flare-ups |
| Social Dining | Research menu ahead; Communicate dietary needs | Minimizes stress and increases enjoyment of social events |
| Emotional Stress | Join GERD support groups; Practice self-care | Provides emotional support and validation |
By developing preemptive coping strategies and cultivating a supportive network, individuals with GERD can navigate their diet with confidence and maintain their regimen without sacrificing their social lives or emotional health. It’s an ongoing process that requires patience and persistence, but it’s a critical aspect of living a full and satisfying life with GERD.
Conclusion
My journey into the world of GERD diets has been marked by a constant search for long-term health with GERD. This path has taught me that embracing dietary changes for GERD is more than a mere short-term fix; it’s a commitment to a lifestyle adjustment that holds profound implications for health and well-being. Foods that treat my gut gently and reduce acid reflux symptoms have offered me relief while also setting the stage for sustainable, healthier living habits.
Embracing Long-Term Health Through Dietary Choices
Adopting a GERD-friendly diet is an act of self-care that extends far beyond immediate symptom control. The choices I make at the dinner table have the power to either soothe or exacerbate my condition. Therefore, learning about acid reflux relief and making informed decisions about the foods I eat is a continuous process that requires patience and persistence. It is a way of life that focuses on nurturing my body and allows for a better understanding of how to achieve and maintain balance within my digestive system.
Encouragement for Continued Learning and Adaptation
I encourage anyone dealing with GERD to remain undeterred in the face of dietary limitations and to continue learning about the intricacies of this condition. Open-mindedness to adapt your eating habits and to try new foods that may offer respite from GERD symptoms is crucial. Embracing this proactive approach can create resilience and a space where physical health is in harmony with one’s emotional state, thus fostering an all-encompassing approach to managing GERD.
FAQ
What is Gastroesophageal Reflux Disease (GERD)?
GERD is a chronic condition where stomach acid frequently flows back into the esophagus, which can lead to symptoms like heartburn, regurgitation, and discomfort.
How does diet play a role in managing acid reflux?
Certain foods can aggravate GERD by relaxing the lower esophageal sphincter or causing delayed digestion. A diet tailored to minimize acid reflux typically includes alkaline foods, lean proteins, and certain vegetables, while limiting trigger foods like fatty meats, spicy dishes, and carbonated beverages.
What lifestyle changes can help alleviate GERD symptoms?
Along with dietary adjustments, lifestyle changes such as eating smaller, more frequent meals, avoiding lying down after eating, elevating the head while sleeping, managing stress, and exercising regularly can reduce the frequency and severity of GERD symptoms.
Which foods can help alleviate the symptoms of acid reflux?
Foods that can help with acid reflux include alkaline foods like bananas and melons, whole grains such as oats and brown rice, lean proteins, green vegetables like broccoli, and root vegetables like sweet potatoes. Herbal teas and broths can also be soothing.
What are some common foods known to trigger GERD symptoms?
Common triggers include high-fat and fried foods, spicy dishes, citrus fruits, tomato-based products, chocolate, caffeine, and alcohol. It’s important to note that triggers can vary from person to person.
How important is meal timing for managing acid reflux?
Meal timing is crucial; eating smaller, more frequent meals and avoiding meals close to bedtime can reduce the risk of acid reflux. It’s recommended to wait at least 2-3 hours after eating before lying down.
Should I consult a healthcare professional to create a GERD-friendly diet?
Yes, consulting with healthcare providers like gastroenterologists can provide valuable insights into creating a personalized GERD diet plan and offer advice on both dietary and medicinal treatments for acid reflux.
What strategies can I use to manage GERD flare-ups and dietary restrictions in social settings?
For managing flare-ups, quickly recognizing symptoms and using strategies such as antacids or a quick walk may be helpful. In social settings, planning ahead, communicating dietary restrictions, and focusing on available food choices can streamline the process and minimize discomfort.
How can I continue to learn about and adapt my diet for long-term health living with GERD?
Stay informed through reputable sources, be open to adjusting your diet as you learn what works best for you, and seek support from healthcare professionals and support groups to help maintain your diet and manage GERD effectively.








Leave a Reply